How AI is Unlocking the Secrets of Your Heart: Game-Changer or Too Soon to Trust?
Can AI outsmart cardiologists, or is it just another tool in the kit?
What if a simple test could predict heart failure before symptoms even appear?
For decades, ECGs have been a cornerstone of cardiac care, but their full potential is only now being unlocked—by artificial intelligence. AI isn’t just improving how we interpret these waveforms; it’s uncovering life-saving insights hidden in plain sight. But with such powerful technology comes big challenges: Can AI be trusted to read your heart’s future? And will it truly revolutionize healthcare, or is widespread adoption still a distant dream? Let’s explore where we are, what’s possible, and what’s holding us back.

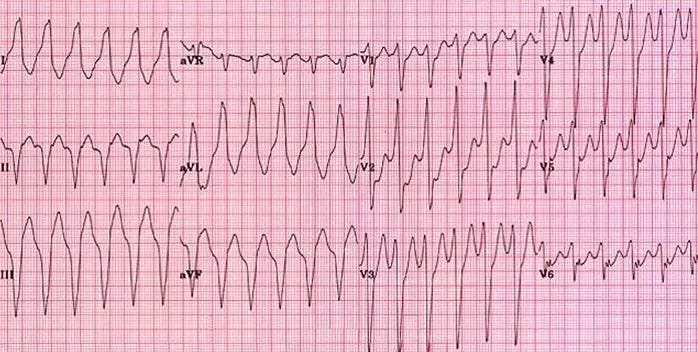
Understanding an ECG in Simple Terms
An electrocardiogram (ECG) is a non-invasive test that records the electrical activity of the heart. By placing electrodes on the skin, it captures the heart’s electrical signals, displaying them as waveforms on a monitor or paper. These waveforms help healthcare providers assess heart rhythm, detect abnormalities, and diagnose various cardiac conditions.
The Importance and Challenges of Interpreting ECGs
ECGs are vital tools in cardiology, essential for diagnosing conditions like arrhythmias, heart attacks, and other heart diseases. However, interpreting ECGs is complex. The subtle variations in waveforms require significant expertise to distinguish between normal and pathological patterns. Even experienced clinicians can find it challenging to interpret ECGs accurately, leading to potential misdiagnoses or overlooked conditions. As a medical student, it is incredibly difficult to learn (from our own experiences).
Landmark Study: AI Unveils Hidden Cardiac Risks
A groundbreaking study published in The Lancet Digital Health demonstrated the potential of artificial intelligence (AI) in ECG analysis. Researchers from Imperial College London developed an AI model trained on millions of ECGs to predict patients’ risk of developing and worsening diseases, including the risk of early death. This model, known as AI-ECG Risk Estimation (AIRE), was able to identify subtle patterns in ECGs that are often imperceptible to human clinicians, enabling early detection of conditions like heart rhythm problems and heart failure.
The Current State of AI powered ECG’s:
Pros and Cons
Pros:
1. Enhanced Diagnostic Accuracy:
AI models demonstrate diagnostic accuracy that is often comparable to or exceeds that of human experts. These models excel in identifying conditions such as atrial fibrillation, left ventricular dysfunction, and coronary artery disease (Makimoto et al., 2020; Huang et al., 2022). A notable example is PMcardio, developed by Powerful Medical, which uses AI to enhance ECG interpretation. The platform has proven to improve diagnostic precision, particularly in detecting nuanced abnormalities that may be overlooked by human interpretation. This technology bridges the gap between expertise and precision, significantly reducing errors and improving outcomes (Powerful Medical Blog).
2. Early Detection of Subclinical Conditions:
By identifying subtle ECG patterns undetectable by human interpretation, AI enables earlier detection of cardiac and non-cardiac diseases. This capability is critical for diagnosing conditions like left ventricular systolic dysfunction before symptoms arise (Attia et al., 2021).
3. Efficiency and Scalability:
AI integration into wearable and mobile devices provides scalable solutions for mass screenings, particularly in resource-limited or remote areas. This approach enhances accessibility to advanced cardiac care and helps bridge healthcare disparities (Sangha et al., 2021).
4. Integration with Multimodal Data:
AI systems can incorporate data from multiple sources, including imaging and genomics, to enhance risk stratification and improve diagnostic accuracy. This multimodal approach supports personalized medicine and comprehensive patient care (Martínez-Sellés & Marina-Breysse, 2023).
5. Real-Time Monitoring:
AI-powered devices offer continuous ECG monitoring, providing real-time alerts to clinicians about significant changes in cardiac status. This immediate feedback enables timely intervention and improves patient outcomes (Siontis et al., 2021).
Cons:
1. Explainability and Trust Issues:
Many AI models function as black boxes, meaning their decision-making processes are not transparent. This lack of explainability makes it difficult for clinicians to fully trust and adopt these tools (Jang et al., 2024).
2. Dependence on Data Quality:
AI performance is highly dependent on the quality and diversity of training datasets. Models trained on limited or biased data may fail to generalize across different patient populations, leading to potential inaccuracies (Di Costanzo et al., 2024).
3. Ethical and Medico-Legal Challenges:
Questions about accountability for AI errors and concerns over patient data privacy remain significant barriers to widespread adoption. These issues necessitate clear guidelines and robust regulatory frameworks (Attia et al., 2021).
4. Barriers to Implementation:
Many healthcare facilities, particularly those in resource-limited settings, lack the infrastructure needed to integrate AI tools into existing workflows. In some cases, paper-based ECG systems are still prevalent, further complicating AI adoption (Bodagh et al., 2023).
5. Potential for Over-Reliance:
Dependence on AI tools could reduce clinicians’ engagement with ECG interpretation, potentially diminishing their diagnostic skills and learning opportunities. Balancing AI use with human expertise is essential (Di Costanzo et al., 2024).
Patient Experiences
1. Improved Accessibility and Early Diagnosis:
• AI-enhanced ECG algorithms have been deployed in routine health check-ups, enabling early detection of conditions like coronary artery disease in asymptomatic patients. This reduces the need for invasive procedures and enhances patient outcomes (Huang et al., 2022).
2. Enhanced Trust in AI for Health Monitoring:
• Patients utilizing mobile devices or wearables with AI-enhanced ECG features have reported confidence in these technologies for continuous health monitoring, especially for conditions like atrial fibrillation (Siontis et al., 2021).
3. Potential Concerns About Misdiagnosis:
• While AI tools improve diagnostic precision, patients have expressed concerns over misinterpretations or false positives, emphasizing the need for human oversight to validate AI findings (Yao et al., 2021).
4. Practical Challenges in Adoption:
• The incorporation of AI in healthcare settings requires patients to adapt to new technologies, such as ECG-enabled stethoscopes. Some patients have faced difficulty understanding how AI influences their diagnosis and treatment (Attia et al., 2022).
5. Positive Impact on Mental Well-being:
• Knowing that AI-enhanced ECGs can predict and prevent severe outcomes like heart failure has been reassuring for patients, particularly those with a history of cardiovascular diseases (Rabinstein et al., 2021).
A Bright Future for AI in ECG Diagnostics
The future of using AI in ECG interpretation is poised to revolutionize cardiovascular care, making diagnostics more precise, accessible, and integrated. AI-enhanced ECG tools are transforming this century-old diagnostic method by uncovering subclinical patterns and integrating with other modalities like imaging and biomarkers to improve disease management and risk prediction (Martínez-Sellés & Marina-Breysse, 2023).
These tools can localize conditions such as coronary artery disease, allowing early intervention and serving as effective screening options during routine check-ups (Huang et al., 2022).
With advancements in mobile and wearable technologies, AI-ECG applications are scalable and capable of providing real-time insights for patients and clinicians alike, democratizing access to care (Attia et al., 2021; Siontis et al., 2021).
However, the road to adoption is not without challenges—stakeholders have identified the need for AI to handle both digital and paper-based ECGs, address transparency in algorithmic decision-making, and ensure explainability for clinician trust (Bodagh et al., 2023; Niemczyk et al., 2024).
Despite these hurdles, ongoing improvements in AI accuracy and versatility suggest a future where ECGs not only diagnose but also predict conditions, enabling preventative interventions and transforming the patient care paradigm (Kashou et al., 2020; Sangha et al., 2021). As AI capabilities continue to evolve, ECG technology is expected to bridge gaps in healthcare delivery, offering unprecedented opportunities for scalable, precise, and proactive cardiovascular diagnostics.
References
1. Attia Z, Harmon D, Behr E, Friedman P. Application of artificial intelligence to the electrocardiogram. Eur Heart J. 2021;42(30):2927-2936. doi:10.1093/eurheartj/ehab649.
2. Huang P, Tseng Y, Tsai C, et al. An artificial intelligence-enabled ECG algorithm for the prediction and localization of angiography-proven coronary artery disease. Biomedicines. 2022;10(2). doi:10.3390/biomedicines10020394.
3. Makimoto H, Höckmann M, Lin T, et al. Performance of a convolutional neural network derived from an ECG database in recognizing myocardial infarction. Sci Rep. 2020;10.
4. Sangha V, Mortazavi B, Haimovich A, et al. Automated multilabel diagnosis on electrocardiographic images and signals. Nat Commun. 2021;13.
5. Siontis KC, Noseworthy PA, Attia ZI, Friedman PA. Artificial intelligence-enhanced electrocardiography in cardiovascular disease management. Nat Rev Cardiol. 2021;18(7):430-444. doi:10.1038/s41569-020-00503-2.
6. Jang JH, Jo YY, Kang S, et al. Unveiling AI-ECG using Generative Counterfactual XAI Framework. Preprint. 2024.
7. Bodagh N, Ali O, Kotadia I, et al. Feasibility of artificial intelligence-enhanced electrocardiogram (AI-ECG) analysis in the current clinical environment: An online survey. Europace. 2023;25(Suppl 3):iii122.533. doi:10.1093/europace/euad122.533.
8. Di Costanzo A, Spaccarotella C, Esposito G, Indolfi C. An artificial intelligence analysis of electrocardiograms for the clinical diagnosis of cardiovascular diseases: A narrative review. J Clin Med. 2024;13.
9. Makimoto H, Attia ZI, Harmon DM, et al. Artificial intelligence-enabled electrocardiograms for prediction of left ventricular systolic dysfunction. The Lancet Digital Health. 2024.
10. Martínez-Sellés M, Marina-Breysse M. Current and future use of artificial intelligence in electrocardiography. J Cardiovasc Dev Dis. 2023;10(4). doi:10.3390/jcdd10040175.
11. Powerful Medical. How is AI transforming ECG interpretation? Published 2024.
12. European Society of Cardiology. Artificial intelligence in ECG diagnostics: where are we now? Published 2023.
13. Imperial College London. AI model can predict health risks, including death, from simple ECGs. Published 2023.
14. American Heart Association News. Can EKGs read by AI save lives? It’s possible, researchers say. Published 2023.
15. Mayo Clinic News Network. AI-enhanced ECG technology shows promise for early diagnosis. Published 2024.
16. Yao X, Rushlow D, Inselman JW, et al. Artificial intelligence–enabled electrocardiograms for identification of patients with low ejection fraction: a pragmatic, randomized clinical trial. Nat Med. 2021;27(6):815-819. doi:10.1038/s41591-021-01335-4.
17. Attia Z, Dugan J, Rideout A, et al. Automated detection of low ejection fraction from a one-lead electrocardiogram: application of an AI algorithm to an electrocardiogram-enabled digital stethoscope. Eur Heart J Digit Health. 2022;3(3):373-379. doi:10.1093/ehjdh/ztac030.
18. Rabinstein A, Yost MD, Faust LJ, et al. Artificial intelligence-enabled ECG to identify silent atrial fibrillation in embolic stroke of unknown source. J Stroke Cerebrovasc Dis. 2021;30(9):105998. doi:10.1016/j.jstrokecerebrovasdis.2021.105998.
19. Kashou AH, May AM, Noseworthy PA. Artificial intelligence-enabled ECG: a modern lens on an old technology. Curr Cardiol Rep. 2020;22(10):105. doi:10.1007/s11886-020-01317-x.
20. Niemczyk S, Fiegler-Rudol J, Migas M, et al. Artificial intelligence in ECG analysis—future or present? Emerg Med Serv. 2024;24(2):106. doi:10.36740/emems202402106.




